Abstract
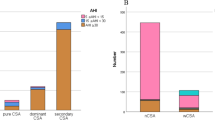
Patients with complex sleep apnea syndrome (CompSAS) have obstructive sleep apnea but develop troublesome central sleep apnea activity or Cheyne–Stokes breathing when provided continuous positive airway pressure (CPAP) therapy. We examined whether CompSAS activity persists with long-term CPAP treatment. We retrospectively identified all patients with CompSAS who underwent two therapeutic polysomnograms (PSGs) separated by at least 1 month during 2003–2005. We compared PSG findings between the initial and follow-up study and noted clinical responses to therapy. We identified 13 CompSAS patients meeting criteria. Most follow-up PSGs were ordered after an abnormal overnight oximetry on CPAP or because of CPAP intolerance after 195 (49–562) days. The residual apnea–hypopnea index (AHI) on CPAP decreased from 26 (23–40) on the first PSG to 7 (3–21.5) on the follow-up PSG. Only seven patients reached AHI < 10 and 6 had AHI ≥ 10 (“CPAP nonresponders”) at follow-up. “CPAP nonresponders” were sleepier (Epworth Sleepiness Score 13 [12.5–14] vs 9 [6–9.5], p = 0.03) and trended toward lower body mass index (29.7 [28.6–31.6] vs 34.3 [32.5–35.1], p = 0.06). Both groups were equally compliant with CPAP therapy. Although the AHI tends to improve over time in CompSAS patients treated with CPAP, in this retrospective study nearly half-maintained a persistently elevated AHI. A prospective trial is merited to determine the optimal treatment for these patients.
Similar content being viewed by others
References
Thomas RJ, Terzano MG, Parrino L, Weiss JW (2004) Obstructive sleep-disordered breathing with a dominant cyclic alternating pattern—a recognizable polysomnographic variant with practical clinical implications. Sleep 27:229–234
Gilmartin GS, Daly RW, Thomas RJ (2005) Recognition and management of complex sleep-disordered breathing. Curr Opin Pulm Med 11:485–493
Morgenthaler TI, Kagramanov V, Hanak V, Decker PA (2006) Complex sleep apnea syndrome: is it a unique clinical syndrome? Sleep 29:1203–1209
Pusalavidyasagar SS, Olson EJ, Gay PC, Morgenthaler TI (2006) Treatment of complex sleep apnea syndrome: a retrospective comparative review. Sleep Med 7:474–479
Ryan CF, Lowe AA, Li D, Fleetham JA (1991) Magnetic resonance imaging of the upper airway in obstructive sleep apnea before and after chronic nasal continuous positive airway pressure therapy. Am Rev Respir Dis 144:939–944
Bradley TD, Logan AG, Kimoff RJ, Series F, Morrison D, Ferguson K, Belenkie I, Pfeifer M, Fleetham J, Hanly P, Smilovitch M, Tomlinson G, Floras JS (2005) Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med 353:2025–2033
Morgenthaler TI, Gay PC, Gordon N, Brown LK (2007) Adaptive servoventilation versus noninvasive positive pressure ventilation for central, mixed, and complex sleep apnea syndromes. Sleep 30:468–475
American Sleep Disorders Association Atlas Task Force (1992) EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 15:173–184
Kales A, Rechtschaffen A (1968) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Brain Information Service/Brain Research Institute, UCLA, Los Angeles, CA
Sahlin C, Svanborg E, Stenlund H, Franklin KA (2005) Cheyne–Stokes respiration and supine dependency. Eur Respir J 25:829–833
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342:1378–1384
Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Javier Nieto F, O'Connor GT, Boland LL, Schwartz JE, Samet JM (2001) Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med 163:19–25
Thomas RJ, Daly RW, Weiss JW (2005) Low-concentration carbon dioxide is an effective adjunct to positive airway pressure in the treatment of refractory mixed central and obstructive sleep-disordered breathing. Sleep 28:69–77
Thomas RJ (2005) Effect of added dead space to positive airway pressure for treatment of complex sleep-disordered breathing. Sleep Med 6:177–178
Acknowledgment
This work was performed with support from Mayo Clinic Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuzniar, T.J., Pusalavidyasagar, S., Gay, P.C. et al. Natural course of complex sleep apnea—a retrospective study. Sleep Breath 12, 135–139 (2008). https://doi.org/10.1007/s11325-007-0140-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-007-0140-z